Hell yes! YES, what we eat directly affects how our gut reacts and how our bowels perform. How could it not?
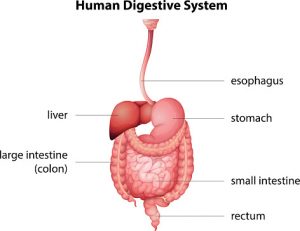
It always blows my mind that doctors ignore diet when treating issues of the stomach and bowels, but that is the current medical standard of care. There is a direct anatomical path from the mouth through the esophagus to the stomach, and then through the intestines to the colon and exiting out through the anus. How could we not recognize that the foods we select to send down that path could be the culprits when it comes to issues along that route such as bloating or gas, cramping or acid reflux, diarrhea or constipation?
A lot of medical research seems to focus almost myopically on the cellular level so much so that doctors can’t see the forest for the trees. According to Dr David Johnson, professor of medicine and chief of gastroenterology at Eastern Virginia Medical School in Norfolk, Virginia, doctors talk to patients “about medication compliance, about taking their tumor necrosis factor (TNF)-alpha antagonists, about immunosuppression, but we rarely talk to them extensively about diet.”
Why is this? Maybe because the concepts of nutrition and diet aren’t covered extensively –or often, not at all– in medical schools, not even for gastro-intestinal specialists. Allopathic doctors are taught to be suspicious of all ideas about health and healthcare that were not presented in medical school or published after large, “Phase 3” placebo-controlled clinical trials, and these are not the best ways to study dietary or nutritional interventions in individuals. Even long-term population-based data on diets can be be misleading because of the impossibility of separating out a single ingredient and correlating it to a health outcome by ignoring the rest of a person’s or population’s food intake. The fields of diet and nutrition have been relegated to the “less-than-doctor” status of Nutritionist or Dietician or even Coach, leading doctors to give food even less credibility when it comes to health.
Or maybe doctors don’t talk to patients about dietary factors because they simply don’t believe in health solutions without pharmaceutical aids. Immunosuppression, or shutting down the immune system’s natural reactions through steroids or other chemical means, is a key medical strategy for addressing gut health issues. It’s tragic because, while steroids can decrease the inflammation and the associated pain, they do not address the root of the problem to begin with.
Even more tragic is the other popular medical solution to continued pain and discomfort along the digestive tract: cut it out. Gallbladders, intestines, colon… you have the right to fight to keep your body intact and functioning! Every part of our body has a function, and once it’s gone, that loss will affect you for the rest of your life. It makes me want to shout from the rooftops: “Before you let someone remove part of your body unnecessarily in order to deal with gut issues, reach out to me and let’s talk about your diet first!”
Dr. Johnson hopes medical officials will start recognizing that “…we have biologic evidence that this makes a difference. It is time for us to start taking a good diet history and treat patients with IBD appropriately. Start looking at diet; it has a key role in the pathogenesis of IBD and may offer a tremendous opportunity in its treatment.”
Dr. Johnson is off to a good start by suggesting that patients with gut dysfunction should begin by eliminating artificial additives and preservatives. He lists carboxymethyl cellulose, polysorbate-80, maltodextrin, and carrageenan as ones to avoid. As I mention in my TEDx talk, these synthetic ingredients are pervasive in our food supply, and avoiding them is easy to do by simply reading labels and learning where they show up most often. I would add food dyes and colors, artificial fragrances, and all artificial sweeteners to this list, along with other chemicals.
Where Dr. Johnson and most other well-meaning doctors fall short is in understanding the best diet to recommend for an individual patient. While he notes that the Mediterranean Diet is preferable to the Standard American Diet, he doesn’t understand that the optimum diet is unique for each individual. This is crucial to understand whether someone is dealing with debilitating gut or bowel function as with Crone’s Disease, or with run-of-the-mill acid reflux or IBS. From my decade of experience designing customized anti-inflammatory diets through my nationwide food sensitivity clinic, I believe the best way to do this is by using the Mediator Release Test (MRT) followed by LEAP Dietary Therapy.
Doctors are uniformly skeptical of this approach (due to the reasons listed above), but I tell them the same thing I tell all of my clients: “You have to eat anyway, so you might as well choose the foods that are not inflammatory for you. What have you got to lose?”
What have you got to lose? In just two weeks you could be feeling markedly better and on the road toward better health, simply by adjusting your food choices.
Contact me for a free initial phone consultation to see if a customized anti-inflammatory diet could help you feel better and live a better life!